Chuncheng Wu, Ping Zhao, Ping Xu, Chaomin Wan, Surjit Singh, Shoban Babu Varthya, Shuang-Hong Luo
Key messages
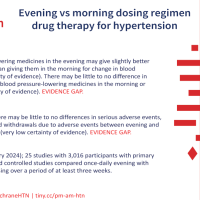
- There may be little to no difference in death for any reason between taking blood pressure‐lowering medicines in the morning or evening, but we have no confidence in the results. The difference in unwanted effects was not known.
- Taking blood pressure‐lowering medicines in the evening may give slightly better blood pressure control than giving them in the morning for change in blood pressure over a 24‐hour period, but we have no confidence in the results.
What is high blood pressure?
High blood pressure (hypertension) is a condition where the pressure inside your arteries is 130 mmHg or greater when your heart is contracting or 80 mmHg or greater when your heart is relaxed, or both of these. The cause of high blood pressure may be unclear or due to some diseases such as kidney disease. People with high blood pressure do not usually have symptoms, but they are at risk for heart attack, stroke and kidney disease.
How is high blood pressure treated?
There are a few ways to help reduce your high blood pressure:
- Take blood pressure‐lowering medicines
- Lose weight (if you are overweight)
- Exercise for at least 30 minutes a day on most days of the week
- Choose a diet low in salt and fat, and rich in fruits and vegetables
- Drink less alcohol (if you drink more than two alcoholic drinks per day)
What did we want to find out?
Does taking blood pressure‐lowering medicines in the evening gave better results than taking them in the morning to improve death, unwanted effects on the heart and blood vessels, unwanted outcomes overall and blood pressure levels?
What did we do?
We searched for studies that compared taking blood pressure‐lowering medicines in the evening with taking them in the morning in people with high blood pressure of unknown cause. We compared and summarised the results of the studies and rated our confidence in the evidence, based on factors such as study methods and sizes.
What did we find?
We found 25 studies including 3016 people with high blood pressure of unknown cause that reported results after three to 26 weeks of treatment with blood pressure‐lowering medicines.
What were the main results?
There may be little to no difference in death from all causes and unwanted outcomes overall, but the evidence was very uncertain. Taking blood pressure‐lowering medicines in the evening may give slightly better blood pressure control than giving them in the morning for change in blood pressure over a 24‐hour period, but we have no confidence in the results. No studies reported unwanted effects on the heart and blood vessels.
What are the main limitations of the evidence?
A few factors reduced our confidence in the evidence. The evidence did not cover many black and Asian people, people with more risks of unwanted outcomes, people taking more than one type of blood pressure‐lowering medicine, people with high blood pressure caused by certain diseases and shift workers. In addition, study durations were less than six months. There were too few studies to be certain about the results of our outcomes. It is possible that the people in the studies were aware of which treatment they were getting, important data may have been lost in the studies, and not all the studies provided data about everything that we were interested in. Finally, results were very inconsistent across the different studies. Our lack of confidence in the results means that further research could change the results in this review.
How up to date is this evidence?
This review updates our previous review. The evidence is up to date to June 2022.
Read the review: Evening versus morning dosing regimen drug therapy for hypertension
Wu C, Zhao P, Xu P, Wan C, Singh S, Varthya SB, Luo S-H. Evening versus morning dosing regimen drug therapy for hypertension. Cochrane Database of Systematic Reviews 2024, Issue 2. Art. No.: CD004184. DOI: 10.1002/14651858.CD004184.pub3. Accessed 16 February 2024.
